Shoulder Tendon Pain
What is a Shoulder Tendon?
The shoulder is a complex joint that is made up of several tendons, muscles, and bones. The tendons in the shoulder connect the muscles to the bones, allowing the joint to move and function properly.
A shoulder tendon is a tough and fibrous band of tissue that connects muscle to bone and can withstand significant tension. Tendons are made of collagen, and together with the muscles, they work to move bones.
Common tendon problems include:
- Tendinopathy
What is Tendinopathy?
Tendinopathy is a medical condition that occurs when the tendons in the shoulder become damaged or inflamed due to repetitive strain or overuse. It is a degenerative disease that affects the tendons connecting the muscles to the bones in the shoulder joint. The tendons in the shoulder joint are responsible for stabilising the joint and allowing for a wide range of motion.
Tendinopathy is also known as tendinosis and tendonitis. Tendinopathy is a broader term than tendonitis and tendinosis, as it refers to any form of tendon injury without defining the type of injury.
Impact of Tendinopathy on Anatomy and Health
Tendinopathy affects the shoulder's anatomy by causing damage to the tendons that connect the muscles to the bones in the shoulder joint. This damage can result in pain, weakness, and loss of range of motion. Over time, untreated tendinopathy can lead to chronic pain and disability, making it difficult for individuals to perform everyday activities.
Who is Most at Risk for Tendinopathy?
Tendinopathy is a condition that can affect anyone, but certain individuals are more at risk than others. Athletes who participate in sports that require repetitive overhead movements, such as tennis, swimming, or baseball, are at a higher risk of developing tendinopathy. Manual labourers, such as construction workers or painters, are also at a higher risk due to the repetitive nature of their work.
Other risk factors include poor posture, shoulder instability, and age-related degeneration. Individuals who are overweight or have a history of shoulder injuries are also at an increased risk of developing tendinopathy.
What are the Causes of Tendinopathy?
Tendinopathy is typically caused by repetitive overhead movements, such as throwing a ball or painting a ceiling, that place excessive strain on the tendons in the shoulder joint.
Tendinopathy Symptoms
The symptoms of tendinopathy may vary from person to person, but the most common ones include the following:
- Pain or tenderness in the shoulder
- Weakness in the shoulder
- Stiffness in the shoulder joint
- Difficulty lifting or moving the arm
- Pain that worsens at night
- Clicking or popping sounds in the shoulder joint
- Swelling or redness around the shoulder joint
You may have more pain and stiffness during the night or when you get up in the morning.
Tendinopathy can affect the following areas:
- Quadriceps
- Achilles Tendon
- Biceps Tendon
Types of Tendinopathy
There are two main types of tendinopathy: acute and chronic.
- Acute tendinopathy is a sudden onset of pain and inflammation in the tendons of the shoulder joint. This type of tendinopathy usually occurs due to a traumatic injury, such as a fall or sudden impact. It can also occur due to a sudden overload or excessive strain on the shoulder joint, such as lifting a heavy object or performing a sudden overhead movement.
- Chronic tendinopathy is a long-term condition that develops gradually over time due to repetitive overhead movements or other forms of overuse. This type of tendinopathy is more common than the acute form and is often seen in athletes, manual labourers, and individuals who perform repetitive overhead movements in their daily activities. Chronic tendinopathy can cause persistent pain, weakness, and loss of function and may require more aggressive treatment options to manage.
What are the Stages of Tendinopathy?
The inability of your tendon to adapt to the load quickly enough causes the tendon to progress through three stages, each with different symptoms and severity:
- Stage 1: Inflammation – The tendon is inflamed and may cause pain and discomfort, particularly during overhead movements. The inflammation can be treated with rest, ice, and medication.
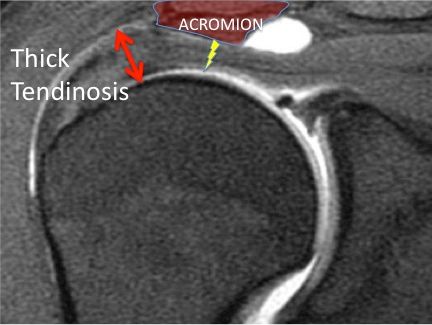
- Stage 2: Tendinosis – The tendon becomes degenerated due to chronic overuse, and the pain may worsen, especially during movement. This stage requires more aggressive treatment, such as physiotherapy, to promote healing and restore function.
- Stage 3: Tendon tear – The tendon is severely damaged in this stage, and a tear may occur. This stage requires surgical intervention to repair or replace the damaged tendon.
Diagnosis of Tendinopathy
Tendinopathy is diagnosed through physical examination, medical history, and imaging tests.
Physical Examination
During the physical exam, the orthopaedic surgeon will:
- Evaluate the shoulder joint's range of motion, muscle strength, and pain or tenderness.
- Perform specific manoeuvres, such as the Neer or Hawkins tests, to assess for signs of impingement or other conditions contributing to the pain.
Medical History
The medical history will help identify any underlying conditions or risk factors that may contribute to the condition's development. The surgeon will ask questions about the onset of symptoms, location and severity of pain, prior shoulder injuries, and underlying health conditions contributing to the tendinopathy.
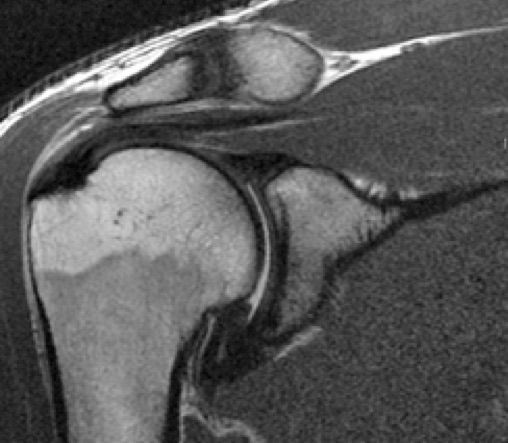
Imaging Tests
Imaging tests such as ultrasound, MRI, or X-ray may be used to understand the nature of any loss in the joint space or bone spur formation.
- X-rays do not show tendons but may show shape changes in the shoulder blade that may narrow the tunnel over the rotator cuff tendons. X-rays also show arthritis of the ball and socket or collar bone/shoulder blade (AC) joint that can also cause should
- Ultrasound can visualise the rotator cuff tendons, compare both shoulders and examine the tendons with arm motion.
- MRI can create detailed images of both hard and soft tissues. An MRI can produce cross-sectional images of internal structures required if the diagnosis is unclear or surgery is being considered.
While not all of these approaches or tests are required to confirm the diagnosis, this diagnostic process will also allow the surgeon to review any possible risks or existing conditions that could interfere with the surgery or its outcome.
Treatment for Tendinopathy
The treatment for tendinopathy depends on the severity of the condition and the stage of the disease. Mild cases can be treated with rest, ice, and medication, while more advanced cases may require physiotherapy, corticosteroid injections, or surgery.
- Rest, Ice, and Medication: In the early stages of tendinopathy, rest, ice, and medication may be recommended to reduce inflammation and relieve pain. Resting the shoulder and avoiding activities that aggravate the pain can help promote healing. Applying ice to the shoulder for 15-20 minutes several times daily can also help reduce inflammation. Over-the-counter pain medication such as ibuprofen or acetaminophen can be used to manage pain.
- Physiotherapy: Physiotherapy is a common treatment for tendinopathy, especially in cases where the condition has progressed beyond the early stages. Physiotherapy involves exercises that aim to strengthen the muscles around the shoulder joint, improve flexibility, and reduce pain. It may also include manual therapy, such as massage or joint mobilisation, to help restore the shoulder joint's normal range of motion.
- Corticosteroid Injections: Corticosteroid injections may reduce inflammation and pain in cases where rest and physiotherapy have not provided relief. These injections can effectively reduce pain and inflammation, but they should be used cautiously as they can cause long-term damage to the tendon.
- Surgery: In severe cases where conservative treatments have failed, surgical intervention may be necessary to repair or replace the damaged tendon. The type of surgery will depend on the extent of the damage, but it may involve removing damaged tissue, repairing the tendon, or replacing the tendon with a graft.
Surgery for Tendinopathy
Surgery for tendinopathy is typically considered when conservative treatments, such as rest, physiotherapy, and medication, have failed to relieve pain and improve function. Surgery is often recommended for individuals with significant damage to the tendons in the shoulder joint, such as a partial or full-thickness tear.
The type of surgery recommended will depend on the extent and location of the damage. Some common surgical procedures for tendinopathy include:
- Arthroscopic Debridement: This procedure involves using a small camera and specialised instruments to remove any damaged tissue in the shoulder joint. This type of surgery is often used for mild to moderate cases of tendinopathy.
- Rotator Cuff Repair: This surgery is typically recommended for more severe cases of tendinopathy, particularly those involving a full-thickness rotator cuff tear. The procedure involves reattaching the damaged tendon to the bone using sutures or anchors.
- Tendon Transfer: A tendon transfer may be recommended in cases where the rotator cuff is severely damaged or unable to be repaired. This procedure involves taking a healthy tendon from another part of the body and using it to replace the damaged tendon in the shoulder joint.
Recovery from surgery for tendinopathy can vary depending on the type of procedure performed and the extent of the damage. Physiotherapy is typically required after surgery to help restore strength, mobility, and function to the shoulder joint. Full recovery can take several months, and it may take up to a year for individuals to regain full range of motion and strength in the shoulder.
What if Tendinopathy is Untreated?
If left untreated, tendinopathy can lead to chronic pain, loss of function, and disability. The condition can worsen over time, leading to more extensive damage to the tendon, which may require more invasive treatments, such as surgery. Untreated tendinopathy can also impact an individual's quality of life, making it difficult to perform everyday activities, such as dressing, driving, or lifting objects.