Practice Locations
Bega Valley Centre for Bone & Joint Surgery Rajesh Orthopaedics
19 Canning St, Bega NSW 2550, Australia
Mogo Day Surgery
Mogo Day Surgery, 2-4 Charles St NSW 2536 Australia
Bombala St Surgery
62 Bombala St, Cooma NSW 2630, Australia
Shoulder Arthritis
What is Shoulder Arthritis?
The term arthritis means inflammation of a joint.
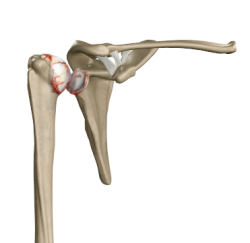
Shoulder arthritis covers numerous conditions where the joint surfaces (cartilage) wear out.
The joint surface is covered by a smooth articular surface that allows pain-free movement in the joint.
The cartilage cushions the bones that make up a joint to absorb stress during movement.
Impact of Shoulder Arthritis on Anatomy and Health
As the cartilage in the shoulder joint wears away, the bones in the joint can rub against each other, causing pain and stiffness. The shoulder joint may also become inflamed, leading to further pain and discomfort. Over time, shoulder arthritis can cause a loss of mobility and function in the shoulder joint, making it difficult to perform everyday tasks such as reaching and lifting.
Who is Most at Risk for Shoulder Arthritis?
Shoulder arthritis is more common in older adults, particularly those over 50. Women are also more likely to develop shoulder arthritis than men. Individuals who have a family history of arthritis, have had previous shoulder injuries or have jobs that require repetitive shoulder movements, such as construction workers or athletes, are also at a higher risk for developing shoulder arthritis.
Causes of Shoulder Arthritis
Damage of the cartilage in the shoulder joint can cause shoulder arthritis.
Numerous conditions can cause arthritis, and sometimes the exact cause is unknown.
When the cartilage is damaged or wears out, the raw bones rub against each, leading to inflammation painfully. The proportion of cartilage damage inflammation varies with the type and stage of arthritis.
Numerous conditions can cause arthritis, and the exact cause is often never known.
- Trauma (fracture)
- Increased stress, e.g., overuse, overweight.
- Avascular necrosis (loss of blood supply)
- Infection
- Growth abnormalities of the shoulder
- Connective tissue disorders
Symptoms of Shoulder Arthritis
The symptoms of shoulder arthritis can vary from person to person but typically include:
- Pain and stiffness in the shoulder joint
- Limited range of motion in the shoulder
- Weakness in the shoulder muscles
- A clicking or popping sensation in the shoulder joint
- Swelling or tenderness around the joint
Types of Shoulder Arthritis
The most common types of arthritis are:
Osteoarthritis
Osteoarthritis, also called wear-and-tear arthritis, is a degenerative joint disease that affects the cartilage.
The cartilage starts to wear away over time, and in extreme cases, nothing remains to protect the bones, causing painful bone-on-bone contact.
Osteoarthritis is the most common type of arthritis, which often occurs with advanced age, excessive strain, or another disease, injury or deformity.

Rotator Cuff Tear Arthropathy
Chronic large rotator cuff tears can cause the shoulder ball to ride high on the socket and rub on the overhanging shoulder blade. This can lead to cartilage wear and painful arthritis characterised by weak, decreased movement.
Rheumatoid Arthritis
Rheumatoid arthritis is an auto-immune disease in which the body's immune system attacks healthy joints. It mostly affects the joints of the hands and feet and tends to be symmetrical (affects the same joints on both sides of the body).
This disease occurs most often in women of childbearing age (15 to 44 years) and inflames the lining of joints (synovium).
With new medications, Rheumatoid disease is better controlled, limiting joint destruction and the need for replacement.
Stages of Shoulder Arthritis
Shoulder arthritis is often a degenerative disease, and the onset increases with age (Osteoarthritis).
Shoulder arthritis typically progresses through four stages, each with increasing severity:
- Stage 1: Minor osteoarthritis characterised by minor cartilage loss and mild symptoms.
- Stage 2: Moderate osteoarthritis with moderate cartilage loss and increasing pain and stiffness in the joint.
- Stage 3: Severe osteoarthritis with significant cartilage loss, significant joint pain and stiffness, and limited range of motion in the joint.
- Stage 4: End-stage osteoarthritis with complete cartilage loss, severe joint pain, and significant joint function loss.
How is Shoulder Arthritis Diagnosed?
Diagnosing shoulder arthritis typically involves a combination of physical exams, medical history, and diagnostic tests. Here are some common diagnostic procedures for shoulder arthritis:
- Physical Exam: The surgeon will start with a physical exam to assess the range of motion in your shoulder and identify areas of tenderness, swelling, or deformity. They will also evaluate your strength and stability in the shoulder joint.
- Medical History: The surgeon will ask about your medical history, including any previous injuries or medical conditions that may be contributing to your shoulder pain.
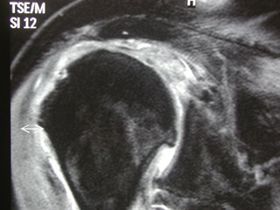
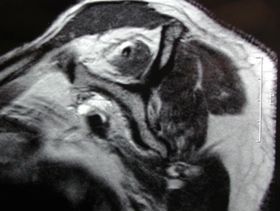
- Imaging Tests: Imaging tests such as X-rays, magnetic resonance imaging (MRI), and ultrasound can help to visualise the joint and identify any structural damage or abnormalities. X-rays can show changes in the joint that may indicate the presence of arthritis, such as narrowing of the joint space, bone spurs, or bone damage. An MRI can provide a detailed image of the joint and may be used to identify cartilage loss or other structural damage. Ultrasound can be used to evaluate the joint's soft tissues, such as the tendons and ligaments.
- Arthroscopy: Arthroscopy is a minimally invasive procedure that involves inserting a small camera into the joint to examine the joint's interior. This procedure can provide a detailed view of the joint, allowing the surgeon to identify any damage or abnormalities contributing to your shoulder pain.
- Laboratory Tests: Blood tests may rule out other causes of joint pain, such as rheumatoid arthritis or infection.
What are the Treatment Options for Shoulder Arthritis?
There is no cure for arthritis, but the symptoms can be managed. Common treatment options include:
- Medications: Over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can help to relieve pain and inflammation. In severe cases, your doctor may prescribe stronger medications or inject corticosteroids directly into the joint.
- Physical Therapy: Physical therapy exercises can help to improve mobility and strength in the shoulder joint.
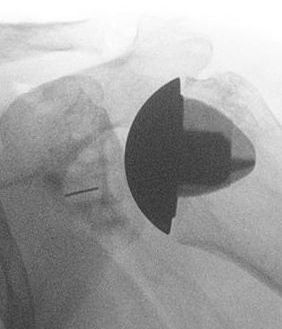
In severe cases of shoulder arthritis, surgery may be necessary. Surgery for shoulder arthritis involves replacing the damaged joint with an artificial joint, which can alleviate pain, improve mobility, and restore function to the joint. There are two main types of shoulder replacement surgeries:
- Total Shoulder Replacement: In total shoulder replacement surgery, the entire shoulder joint is replaced with a prosthetic joint made of metal and plastic. This surgery is typically recommended for patients with severe arthritis in the joint and those who have had a previous shoulder injury or surgery.
- Reverse Shoulder Replacement: In a reverse shoulder replacement surgery, the normal ball-and-socket joint of the shoulder is reversed, with the ball and socket switching positions. This surgery is typically recommended for patients with a rotator cuff tear, as it allows the deltoid muscle to take over the function of the rotator cuff muscles.
Both shoulder replacement surgeries are typically performed under general anaesthesia with a nerve block, usually taking 1-2 hours to complete. After surgery, patients typically need to stay in the hospital for 1-2 days and wear a sling to support their arm for several weeks. Physical therapy will also be required to help regain strength and mobility in the shoulder joint.
While shoulder replacement surgery can be highly effective at relieving pain and improving function in the shoulder joint, it is important to discuss the risks and benefits of the procedure with your doctor before making a decision. Risks associated with shoulder replacement surgery include infection, bleeding, nerve damage, and prosthesis failure. However, for many patients with severe shoulder arthritis, surgery may be the best option to regain mobility and improve their quality of life.


All Rights Reserved | Dr Krishnankutty Rajesh | Privacy